Improving discharge planning and guidance for preterm newborns: Communication challenge
Introduction
Premature births are a significant public health issue, affecting over 14 million births each year worldwide and contributing to 35% of all neonatal deaths. Brazil has the ninth highest rate of prematurity in the world. As preterm birth is primarily linked to socioeconomic and demographic factors, obstetric history and mother-foetal conditions during pregnancy, there is a correlation between prematurity and socially disadvantaged groups. Consequently, social and health inequalities need to be prioritised in public policy. Advances in obstetric and neonatal medicine have significantly increased the survival of preterm infants. However, due to their immature development, preterm babies often experience multiple complications after birth, leading to long-term morbidities among survivors and potential permanent sequelae. This highlights the need to assess and implement care and guidelines to prevent short-term adverse complications and optimise long-term outcomes.
Background
Readiness for discharge of preterm babies is determined by functional maturity rather than weight or corrected gestational age. The hospital team also assesses parents’ involvement, preparations, resources for the baby’s homecoming and planning for follow-up care to monitor the infant’s development. The hospital team can facilitate a smooth transition by enhancing parents’ knowledge and skills in preterm infant care and improving discharge readiness. An individualized discharge plan can enhance patient outcomes and reduce healthcare costs by preventing prolonged hospital stays and strengthening arrangements for subsequent medical and social care.
The problem
In the Neonatal Unit at the University Hospital of São Paulo’s Teaching Hospital, care for preterm newborns is delivered by a multidisciplinary team. However, documentation is fragmented, making it difficult to obtain a clear view of the patient’s care. Discharge instructions are also long and incredibly detailed, which makes recording time-consuming. An overload of information is delivered within a short period of time and in an inappropriate setting where distractions may compromise understanding. Standardising this process could improve both time management and the quality of information provided to families, leading to enhanced readiness for hospital discharge.
The search for answers
To address these issues, we conducted a best practice implementation project to improve discharge planning and guidance for families of preterm newborns. This involved standardising documentation, improving communication and unifying discharge guidance provided to families. Our project used the JBI Evidence Implementation Framework, which is grounded in an audit, feedback and re-audit strategy. The project was coordinated by a multidisciplinary leadership team, including a staff nurse and head nurse from the Neonatal Unit, the director of the Obstetric and Gynaecological Nursing Division, physicians from the outpatient follow-up clinic and the head of the Neonatology Department.
Result/outcome
The project team analysed the existing workflow related to discharge planning and guidance for preterm newborns through a baseline audit. The team then identified modifiable and non-modifiable barriers related to behaviour, service structure, and resource availability. Based on this analysis, the team designed strategies and planned actions to overcome the identified barriers. The core of the improvement strategies was the development of a Discharge Planning Guideline for Preterm Newborns, considering both the scientific literature and an analysis of the unit’s routines and care logistics.
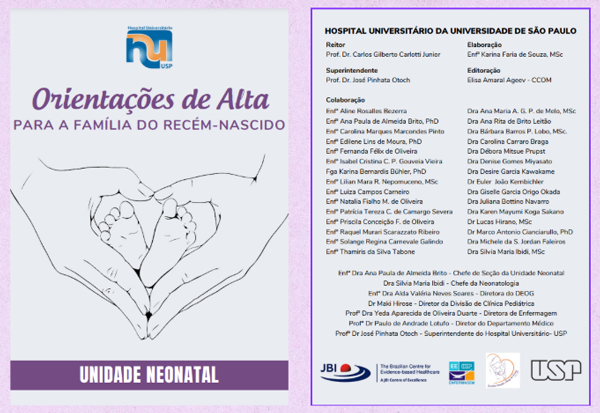
An illustrated booklet with standardised instructions written in plain and easy-to-understand language was also developed. This educational resource was adopted as part of the discharge process.

An existing form was also adapted to allow multidisciplinary teams to document their specific contributions related to discharge assessments and guidance.
 The purpose of this strategy was to improve the organisation of information, thereby making the overall evaluation process more efficient, clear, concise and evidence-informed.
The purpose of this strategy was to improve the organisation of information, thereby making the overall evaluation process more efficient, clear, concise and evidence-informed.
The content of the guideline, the new form and the illustrated booklet were presented to the multidisciplinary teams as standard operating procedures, flowcharts and an educational video developed using AI. The project also used WhatsApp to disseminate the new changes.
A follow-up audit showed improvements, particularly with regard to the discharge planning practices and guidance for families of preterm newborns. The collaborative efforts of the project leads and stakeholders facilitated the implementation process.
Challenges and lessons learned
The University of São Paulo’s Teaching Hospital used a pioneering approach to discharging patients. The project used a comprehensive summary that could be referenced if medical attention was required at another healthcare facility. The project also demonstrated that using educational videos is effective for raising team awareness of the care plan and disseminating the content of guidelines. Nonetheless, a robust sustainability strategy is required to maintain the changes that were introduced.
Next steps
Plans for future audits and strategies for sustainability are being developed to support positive outcomes in the medium and long term.
Key take-home messages
Collaborative communication is key to the success of evidence-informed implementation projects.
The JBI Evidence Implementation Framework is a valuable resource that facilitates the implementation of best practices.
References
Campbell F, Salam S, Sutton A, Jayasooriya SM, Mitchell C, Amabebe E, Balen J, et al. Interventions for the prevention of spontaneous preterm birth: a scoping review of systematic reviews. BMJ Open. 2022;12(5):e052576. http://doi.org/10.1136/bmjopen-2021-052576
Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petsold M, Hogan D, et al. Global, regional and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health 2019;7:E37–E46. https://doi.org/10.1016/S2214-109X(18)30451-0
Gonçalves-Bradley DC, Lannin NA, Clemson L, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2022;2(2):CD000313. http://doi.org/10.1002/14651858.CD000313.pub6
Hua W, Wang L, Li C, Simoni JM, Yuwen W, Jiang L. Understanding preparation for preterm infant discharge from parents' and healthcare providers' perspectives: Challenges and opportunities. J Adv Nurs. 2021;77(3):1379-90. http://doi.org/10.1111/jan.14676
Humberg A, Fortmann I, Siller B, Kopp MV, Herting E, Göpel W, et al. Preterm birth and sustained inflammation: Consequences for the neonate. Semin Immunopathol. 2020;42(4):451-68. http://doi.org/10.1007/s00281-020-00803-2
Jefferies AL, Canadian Paediatric Society, Fetus and Newborn Committee. Going home: Facilitating discharge of the preterm infant. Paediatr Child Health. 2014;19(1):31-42.
Khandre V, Potdar J, Keerti A. Preterm birth: An overview. Cureus. 2022;14(12):e33006. http://doi.org/10.7759/cureus.33006
Leal MD, Esteves-Pereira AP, Nakamura-Pereira M, Torres JA, Theme-Filha M, Domingues RM, et al. Prevalence and risk factors related to preterm birth in Brasil. Reprod Health. 2016;13(Suppl 3):127. http://doi.org/10.1186/s12978-016-0230-0
Magtoto LS. Evidence summary. Premature infants (discharge): Family readiness facilitation. The JBI EBP Database. 2021; JBI-ES-3337-3.
Mitrogiannis I, Evangelou E, Efthymiou A, Kanavos T, Birbas E, Makrydimas G, et al. Risk factors for preterm birth: an umbrella review of meta-analyses of observational studies. BMC Med. 2023;21(1):494. http://doi.org/10.1186/s12916-023-03171-4
Porritt K, McArthur A, Lockwood C, Munn S, editors. JBI Handbook for Evidence Implementation. JBI, 2020. Available from: https://implementationmanual.jbi.global
Porritt K, McArthur A, Lockwood C, Munn S. JBI's approach to evidence implementation: A 7-phase process model to support and guide getting evidence into practice. JBI Evid Implement 2023;21(1):3-13. http://doi.org/10.1097/XEB.0000000000000361
Walani SR. Global burden of preterm birth. Int J Gynaecol Obstet. 2020;150(1):31-3. http://doi.org/10.1002/ijgo.13195
Whitehorn A, Ortega-Arroyo A. Evidence summary. Discharge planning (acute care): Key principles. The JBI EBP Database. 2024; JBI-ES-2779-6.
Younes S, Samara M, Al-Jurf R, Nasrallah G, Al-Obaidly S, Salama H, et al. Incidence, risk factors and outcomes of preterm and early term births: A population-based register study. Int J Environ Res Public Health. 2021;18(11):5865. http://doi.org/10.3390/ijerph18115865
To link to this article - DOI: https://doi.org/10.70253/IMSX6200
Links to additional resources
doi.org/10.17605/osf.io/r4s7b
Co-publication declaration
This project was undertaken as part of the JBI Evidence Implementation Training Program, which was funded by the Brighter Futures Grant Program.
This best practice implementation project has been submitted to the JBI Evidence Implementation journal (no peer review feedback yet).
Disclaimer
The views expressed in this World EBHC Day Blog, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.
