AHRQ’s Evidence-based Practice Center Program: 25 years of partnerships to support evidence-based healthcare
The 25th June 2022 marked the 25th anniversary of the Agency for Healthcare Research and Quality’s (AHRQ) Evidence-based Practice Center (EPC) Program, and there is much to celebrate. The program was designed to support healthcare quality in the United States by providing clinicians, healthcare systems, payers, professional societies and federal partners with the most up-to-date scientific information available to inform high-priority healthcare decisions. The program has stayed true to its mission, and the results of these investments speak for themselves.
Over the last quarter century, the EPC Program has completed over 800 comprehensive systematic reviews of the scientific literature, addressing the needs of more than 100 unique partners. One-third of our partners have been in the U.S. Government, including Congress, agencies in the Department of Health and Human Services (such as the National Institutes of Health [NIH] and the Centers for Medicare and Medicaid Services [CMS]), and other federal entities, such as the Departments of Agriculture, Transportation and Veterans Affairs. The remaining two-thirds of our partners have been in the private sector, most notably professional societies (such as the American College of Physicians and American College of Obstetricians and Gynecologists), and healthcare systems (such as Kaiser Permanente and Intermountain Healthcare).
Despite the depth and heft of the reports we’ve developed, they have not collected dust. For our partners, that would be unacceptable. Our reports have received notice in the halls of Congress, fuelled discourse of lively guideline panels, informed coverage deliberations by payors, shaped research funding notices, and supported decisions about healthcare delivery by C-suite executives nationally. They’ve been the critical evidentiary piece of the puzzle that is evidence-based decision-making (see Figure 1).
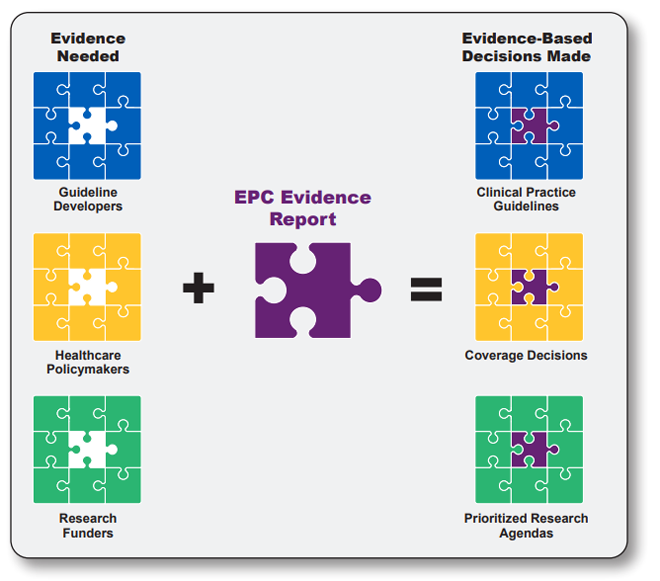
EPC, Evidence-based Practice Center.
Figure 1. Solving the puzzle for evidence-based decision-making
At the birth of the EPC Program, Congressman John Porter noted, while serving on the U.S. House Committee on Appropriations, that: “What we really want to get at is not how many reports (are) done, but how many people's lives are being bettered by what has been accomplished. In other words, is it being used, is it being followed, is it actually being given to patients?” The answer to that question is a resounding “Yes!”
The AHRQ’s evidence reviews have been used by our partners to inform more than:
- 200 clinical practice guidelines issued by federal and professional society partners, including the management of attention-deficit/hyperactivity disorder (ADHD) in children by the American Academy of Pediatrics, opioid prescribing by the Centers for Disease Control and Prevention (CDC), and treatment of post-traumatic stress disorder by the American Psychiatric Association
- 200 U.S. Preventive Services Task Force (USPSTF) guidelines
- 35 national coverage determinations by CMS, including those to cover acupuncture, PET scans, and continuous positive airway pressure (CPAP) for obstructive sleep apnoea
- 40 research prioritisation meetings by the NIH, including those informing research agendas for topics as diverse as hydroxyurea for sickle cell disease, management of viral hepatitis and suicide prevention.
Understanding and disseminating information on these topics is fundamental to improving healthcare in America. Partnerships have been the bedrock of this work, and partners have been essential to defining the highest priority challenges to address up front, providing insight to guide the work, and ensuring the work informs policy and practice to ultimately improve health outcomes.
As a pillar in its long-standing commitment to collaboration, the EPC Program has sought nominations for reviews from diverse stakeholders in healthcare, and has worked tirelessly to identify, build, nurture and sustain relationships with partners whose knowledge and expertise broaden the program’s impact. AHRQ’s efforts to reach beyond its walls have led to important innovations, including stakeholder input throughout the entire evidence-review process to ensure the relevance and usefulness of reports; methods refinements to better incorporate the perspectives of patients and providers in our reviews (such as through the use of qualitative evidence); the development of tools to engage potential end-users (such as through the use of interactive visual dashboards and infographics); approaches to identify and collaborate with partners most in need (such as our recent work with Learning Healthcare Systems); and technologies to streamline the review process and reduce research waste (including the Systematic Review Data Repository, an online open access tool to facilitate the conduct and updating of reviews).
As we begin the EPC Program’s next quarter century, both challenges and opportunities await. The EPC Program is poised to address the following.
- Fostering equity and addressing healthcare needs of the community more broadly. We must build and sustain relationships with partners whose needs have been inadequately addressed and whose expertise has been insufficiently utilised. A greater emphasis on meeting the needs of historically marginalised communities will broaden our perspective and help ensure AHRQ’s reviews support improved healthcare outcomes for all.
- Timeliness of evidence reviews. With the pace of evidence generation and the resulting overflow of information (today’s ‘infodemic’), we need to leverage artificial intelligence, rapid review methodologies and living and evolving reviews to work smarter, not harder. Efficient evidence synthesis production can help provide timely, high-quality information to inform the urgent healthcare decisions of our partners.
- Capitalising on new forms of evidence. Not all answers can be found in well-controlled trials in the scientific literature. At the same time, opportunities to leverage ‘big data’, such as from electronic health records, are rapidly expanding. We need to harness this real-world data to inform and supplement our evidence syntheses, and to ensure our work remains current and actionable.
- Connecting with the evidence ecosystem. We must enhance our evidence ecosystem and help providers more easily deliver and learn from evidence-based care by connecting real-world data with evidence syntheses, evidence syntheses with guideline recommendations, and guideline recommendations with decision support at the point of care.
- Filling gaps for unanswered questions. We need to prioritise identified evidence gaps and more systematically feed those prioritised gaps back to research funders, such as the NIH, to increase research impacts and reduce research waste.
For 25 years, AHRQ’s EPC Program has provided clear, reliable syntheses of the scientific evidence on healthcare topics of the highest priority to policymakers, industry leaders, clinicians and their patients. We will continue to seek and sustain partnerships with end-users, both nationally and globally, as an essential component to helping the nation advance the quality of care in the next quarter century and beyond.
Authors
Craig A. Umscheid, MD, MS1, Christine S. Chang, MD, MPH1.
1. Evidence-based Practice Center Division, Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services
Disclaimer
The views expressed in this World EBHC Day Blog, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.
