Improving mothers’ experience of childbirth through evidence-based intrapartum care
Luciana Magnoni Reberte Gouveia is a professor in the Department of Maternal-Infant and Psychiatric Nursing, at the University of Sao Paulo School of Nursing.
‘In 2018, when I joined the university, I participated in an event organised by the JBI Brazilian Centre for Evidence-Based Healthcare where I learned about the evidence-based projects implemented by researchers who participated in the JBI Evidence Implementation Training Program (formerly the JBI Evidence-Based Clinical Fellowship Program)’, says Luciana.
‘I was so excited to be in an atmosphere in which evidence was being integrated into clinical practice through the efforts and contribution of nurses. The following year I was able to participate in the six-month training program and contribute to improving the model of care for women during childbirth.’
Abuse and disrespect in childbirth care has been deemed a public health issue in Brazil, with many studies documenting the prevalence of discriminatory and hostile attitudes in childbirth care, both in the public and the private sectors.1 Only 5.6% of Brazilian women have normal births without inappropriate and excessive invasive (often not informed or consented to) interventions during vaginal birth,2 such as the unregulated use of oxytocin to induce or augment labour, Kristeller manoeuvre, forceps and episiotomy, among others, often leading to poor obstetric outcomes.1
The nursing professionals, residents and students at the obstetric centre of a teaching hospital in Sao Paulo, where Luciana taught, were dissatisfied with the care they were providing to women in labour. Complaints included inadvertent use of interventions, a care model centred on medical professionals, divergent behaviours and a lack of space for nurses’ and midwives’ autonomy.
Nurses at the teaching hospital observed the need to work with different aspects of obstetric care, with a view to promoting respectful and qualified care for mothers during labour. Luciana focused her six-month JBI evidence-implementation project on improving intrapartum care to improve mothers' experience of childbirth.
‘Women must be the protagonist of their own birth experience, and the teaching and learning process should take place in a respectful environment for mothers and babies’, says Luciana.
Using the JBI Getting Research into Practice (GRiP) approach and the JBI Practical Application of Clinical Evidence System (PACES) audit and feedback tool, a baseline clinical audit measured the following 20 JBI evidence-based audit criteria for best-practice intrapartum care:
1. Effective communication
2. Companion of choice
3. Partograph
4. Not offered routine amniotomy or oxytocin
5. Digital vaginal examination
6. Intermittent auscultation of the foetal heart rate
7. Routine perineal/pubic shaving prior to giving vaginal birth
8. No enema
9. Pain relief options
10. Oral fluid and food intake
11. Mobilize and adopt an upright position
12. Follow their own urge to push
13. No manual fundal pressure
14. Active management of third stage
15. Cord clamp
16. Skin-to-skin contact
17. Vitamin K after one hour
18. Delay bathing of the baby
19. Debriefing opportunities
20. Training every year about intrapartum care
The baseline audit was carried out by a research team, with 27 mothers who had normal births accompanied by obstetric nurses. Compliance with the 20 criteria ranged from <50% for criteria 6 and 19; <75% for criteria 4, 5, 9, 10; <100% for criteria 3, 11, 12, 13, 15, 16, 20; and 100% compliance for criteria 2, 7, 8, 14, 17, 18.
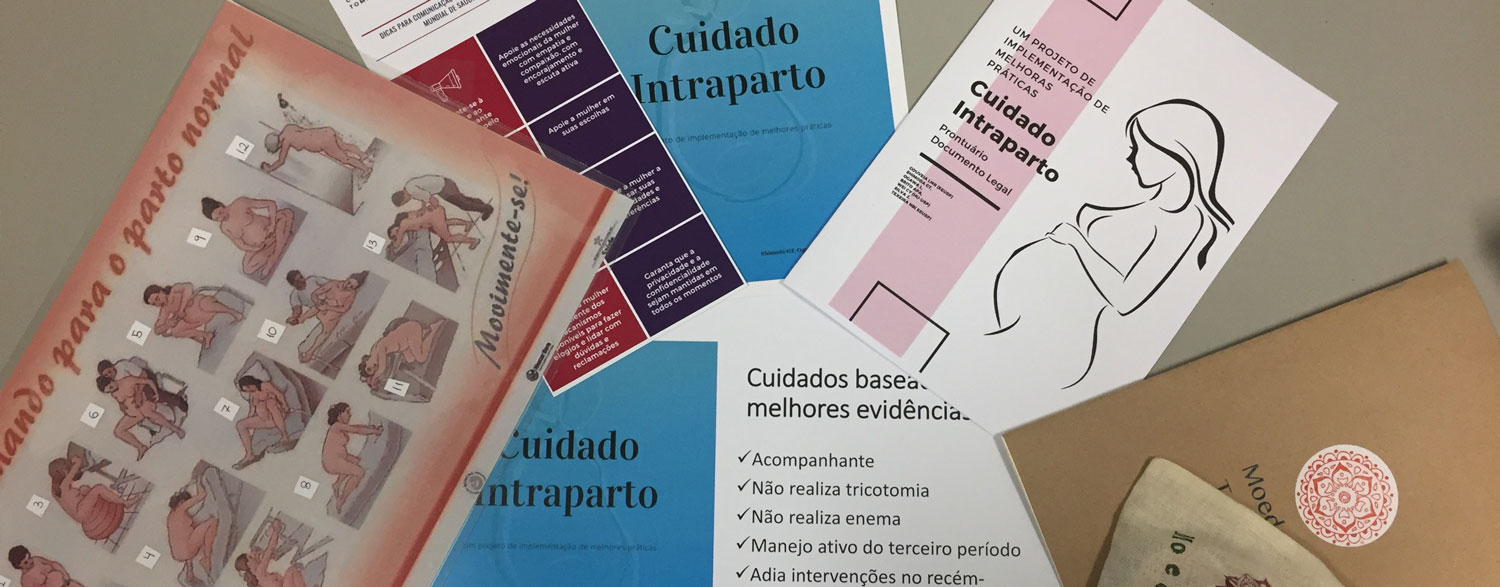
The GRiP phase identified the need i) to conduct in-service training for maintaining accurate nursing records for intrapartum care, reducing interventionist practices and establishing debriefing as a practice; ii) to establish a Game of Values to enable positive reinforcement of service practices and highlight effective communication and respectful maternal care; and iii) for educational pamphlets to improve communication channels for women’s feedback on care.
In total, 30 nursing professionals enrolled in the training and three pamphlets on best practices were developed and delivered. During the in-service training, the Game of Values was used to enable exercises in empathy, dialogue and conflict resolution by following different human values, such as love, generosity, equality, loyalty, joy, respect, balance and dignity, with nurses reflecting on how they practised those values in their daily care.
Through this daily exercise, nurses were also able to reflect on their beliefs that hindered optimal intrapartum care: ‘In relation to the lack of acceptance by the medical team for humanising childbirth, in my head I didn't think I was committing obstetric violence, I thought it was helping.’
Values were practiced in different situations in caring for women during childbirth. For example, love is practiced through bonding, with pain relief measures, guidance, empathy, showing interest, offering support, being together, caring, patience and attention. Employing the Game of Values in this way motivated nurses to adopt and implement the evidence-based practices taught in training, leading to significant improvements in intrapartum care at the teaching hospital.
The follow-up audit demonstrated an improvement in 10 criteria. Most notably, the use of the partograph during labour (3) increased by 20%, compliance with women not being offered routine amniotomy or oxytocin (4) increased by 39%, women being offered pain relief (9) increased by 40% and mothers and babies being given skin-to-skin contact (16) increased by 21%. Moreover, five of the six criteria that achieved 100% compliance in the baseline audit maintained their score.
‘The success of this project was an important step in furthering the collaboration and commitment of the health professionals in the obstetric centre to humanise the childbirth experience for mothers and deliver optimal intrapartum care’, says Luciana.
Challenges for the future include establishing a birthing centre led by nurses and midwives where there is a collaborative exchange environment for health professionals that is led by core human values in delivering quality, evidence-based intrapartum care.
Further Resources
JBI Manual for Evidence Implementation (for GRiP approach)
JBI Practical Application of Clinical Evidence System (PACES)
Authors
Luciana Gouveia, Juliana da Silva, Nathalia Bizari and Pamela Nakazone

References
1. Diniz SG, Salgado HO, Andrezzo HFA, Carvalho PGC, Carvalho PCA, Aguiar CA, Niy DY. Abuse and disrespect in childbirth care as a public health issue in Brazil: origins, definitions, impacts on maternal health, and proposals for its prevention. J Human Growth Dev. 2015;25(3):377-84.
2. Leal MsC, Pereira APE, Domingues RMSM, Filha MMT, Dias MAB, Nakamura-Pereira M et al . Obstetric interventions during labor and childbirth in Brazilian low-risk women. Cad. Saúde Pública. 2014;30 (Suppl 1):S17-S32.
Disclaimer
The views expressed in this this World EBHC Day Impact Story, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.