Increasing capacity to prevent patient falls in an acute care inpatient setting

Patient safety is a multifactorial issue and a benchmark of quality nursing care. One patient safety issue that many institutions have challenges with is preventing patients from falling. There are a variety of interventions to address falls and often a multi-modal approach is needed to keep patients safe. One particular intervention that has been shown to decrease fall rates and decrease safety attendant (SA) utilisation is the utilisation of a remote video monitoring (VM) system. A VM system provides staff the ability to continuously observe select high- risk patients and is a safety strategy utilised in some hospital settings. Systems are equipped with two-way speakers, one-way video, and alarms which enable staff to intervene upon unsafe behaviour to prevent injuries including falls.
Lauren Frahm was a direct care clinical nurse when she started this project at the University of California, San Francisco (UCSF), United States, a large quaternary academic medical centre within the University of California system. UCSF Health provide services ranging from primary care to organ and bone marrow transplants to intensive care for newborns. The hospitals within the system have over 1,000 inpatient beds, have over 750,000 clinic visits annually, with approximately 30,000 patients admitted to the hospitals each year.
Lauren is currently a clinical nurse educator within the Institute for Nursing Excellence (INEx). She was sponsored by INEx to participate in the JBI Evidence Implementation Training Program (formerly the JBI Evidence-Based Clinical Fellowship Program) to develop the knowledge and skills to lead a rapid cycle, small test of change in a clinical setting. Lauren’s six-month evidence-implementation project aimed to ensure continued safety for patients while reducing the need for safety attendants through the introduction of a nurse-led VM system, to increase the number of patients that could be safely monitored.
Studies have determined that in comparison with VM, the safety benefits of utilising SAs were negligible, and therefore VM may be used as a safe alternative that has potential to save resources (Davis & Whyte, 2017). Effective implementation of VM systems in hospital settings include creation of policies and procedures which provide algorithms for appropriate patient selection for monitoring as well as staff education programs (Cournan et al, 2018). However, there is a gap in the literature regarding evidence-based protocols for initiating and discontinuing video monitoring.
Based on JBI best practice recommendations, the project aimed to: (i) Develop a decision-making algorithm for patient selection for video monitoring, (ii) Educate nurses on the three project units regarding use of the VM algorithm, and (iii) Assess nurses’ compliance with best practice criteria, that is, the use of the VM algorithm for initiation and discontinuation of VM.
‘The nurses in the three medical-surgical units selected were not equipped to make evidence-based decisions on choosing the intervention of safety attendant or video monitoring. Safety attendant use is not only costly but having safety attendants in one room takes away help for other patients and staff’ says Lauren.
Therefore, as part of her project Lauren developed an evidence-based tool algorithm for appropriate patient selection for VM and a comprehensive staff education program.

‘There were close to 300 staff on the project units, who had never used video monitoring. So, they needed education about use of the algorithm, but also use of the technology itself. There were a limited number of trainers available and a limited timeframe. Our education strategy was to create and post an e-Learning module with case studies to the hospital’s intranet. The project team also conducted 1:1 training with staff on day and night shifts for a week and tip-sheet reminders were created and posted at nursing stations’ Lauren says.
The staff at first were hesitant to use video monitoring as an intervention and one unit in particular was not engaged in the education of video monitoring use. Lauren addressed these barriers by speaking with staff at huddles, sending email reminders, and speaking with staff individually.
A multimodal education strategy was deployed and included an e-Learning presentation with case scenarios which was posted on the hospital’s intranet, discussion at staff meetings and one-on-one instruction to nurses. Tip-sheets were also created and posted on the units and staff were given verbal and text reminders to document use of the algorithm. Due to limited evidence, Lauren did an extensive literature search to find resources available to guide VM use.

Aggregated results from all three units revealed compliance with initiating video monitoring was highest (79%) during the first post- implementation follow-up audit but decreased to 50% by the third post-implementation audit. Conversely, compliance with discontinuing of VM according to the algorithm increased from 50% at follow-up audit one to 71% at follow-up audit three. By the end of the project, a total of 61% of staff had received education on the use of the VM algorithm and 16 staff members viewed the e-Learning presentation. Five of six nursing supervisors received training on the triage process. Furthermore, there was no increase in falls rates across the project units post intervention of VM algorithm for the following two months, meanwhile hours of safety attendant utilisation decreased by an average of 30%.

This project demonstrated that VM could be just as effective as SA as an intervention to prevent falls in the hospital. As a result of this project, more patients were able to be monitored and safety attendants were appropriately assigned to caring for individual patients.
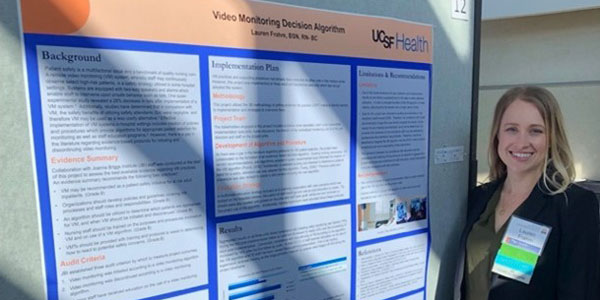
Lauren presented this work at UCSF’s 2020 Clinical InQuERI Conference, where this was broadly shared to a national audience. Hospital policies and procedures were also updated to reflect VM versus SA use for patients in the clinical setting. Safety Attendants were now available to assist with more patients on the units versus sitting in one patient’s room. Research was also conducted to investigate adverse patient outcomes (specifically falls) pre- and post- intervention, as well as across various clinical settings.

With the project’s success being sustained in the three units after completion, and due to the current COVID-19 pandemic where direct interactions with some patients are limited, VM is now being implemented hospital-wide at UCSF. This project now has broader implications where staff are being protected from lengthened exposure, as well as protecting patients while in the hospital.
Further Resources
https://www.ucsfnursing.org/ucsf-jbi-centre
Authors
Lauren Frahm1, Adam Cooper1, Hannah Jang1
1. University of California, San Francisco, San Francisco, CA USA
UCSF Centre for Evidence Synthesis & Implementation: A JBI Centre of Excellence
Disclaimer
The views expressed in this this World EBHC Day Impact Story, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.