Pain Control in Malignant Fungating Wounds
The oncology centre at Cruz Azul Hospital in Sao Paulo, Brazil, attends to approximately 100 patients daily, most of which are military professionals and their families. Suzana Aparecida da Costa Ferreira has worked at the centre as an oncology nurse for eight years, and was also part of the wound care team.
‘One of the biggest challenges in working with patients with cancer is symptom control of malignant fungating wounds (MFW) – injuries where the cancer cells invade the skin or the tumour overgrows, breaking it. MFW are considered a complication of cancer progression, being more present in patients with breast or head and neck neoplasms’, reports Suzana.1,2
Malignant fungating wounds are fragile, exudative, foetid and very painful lesions that negatively impact people's quality of life.3,4,5 Quality of life is impacted due to the number of clinical interventions required, changes in the patient’s daily routine and social isolation. ‘The suffering is extended to the family members due to the anguish at witnessing their loved ones' illness, mixed with the uncertainty of the future’, says Suzana.
Studies show that 100% of patients with MFW have wound-related pain, most of them from moderate to severe intensity.6,7,8 ‘I recall vividly two cases of women with MFW from breast cancer who, despite the use of medication, reported pain at levels of six to eight on the numerical verbal scale (from zero to 10). They would tell me: “This pain is endless, even using morphine…I am always irritated…I lose patience easily and can’t do my daily activities as I would like to do...” and “I’m in a lot of pain, the painkillers I’m taking are not enough… I’m afraid to increase the doses… I also can’t sleep because pain is more intense at night so I’m always tired”.’
At the time, the centre did not have any evidence-based institutional protocols for MFW topical care, and the Brazilian oncological guidelines (INCA, 2009) recommended the use of opioids and topical anaesthetics, without any specific details. Suzana decided to investigate which evidence-based topical therapies could be used for pain relief in MFW.
‘It must be considered that the bioavailability of systemic opioids is unpredictable for the control of pain associated with MFW due to the higher vascular perfusion of the MFW and in the surrounding skin.9 These substances are frequently applied in clinical practice, although not always supported by the best scientific knowledge, as shown by some reviews.’ 10,11,12

Suzana’s first step was to join the Stomal Therapy Nursing Research Group (GPET) of the University of Sao Paulo, School of Nursing (EEUSP), a group is focused on conducting research and dissemination through publications, events and on social media to reach health professionals and also the general public. She then completed the Comprehensive Systematic Review Training Program at The Brazilian Centre for Evidence-based Health Care: A JBI Centre of Excellence to prepare her for conducting a scoping review on the best available evidence on topical therapies for pain relief of MFW.
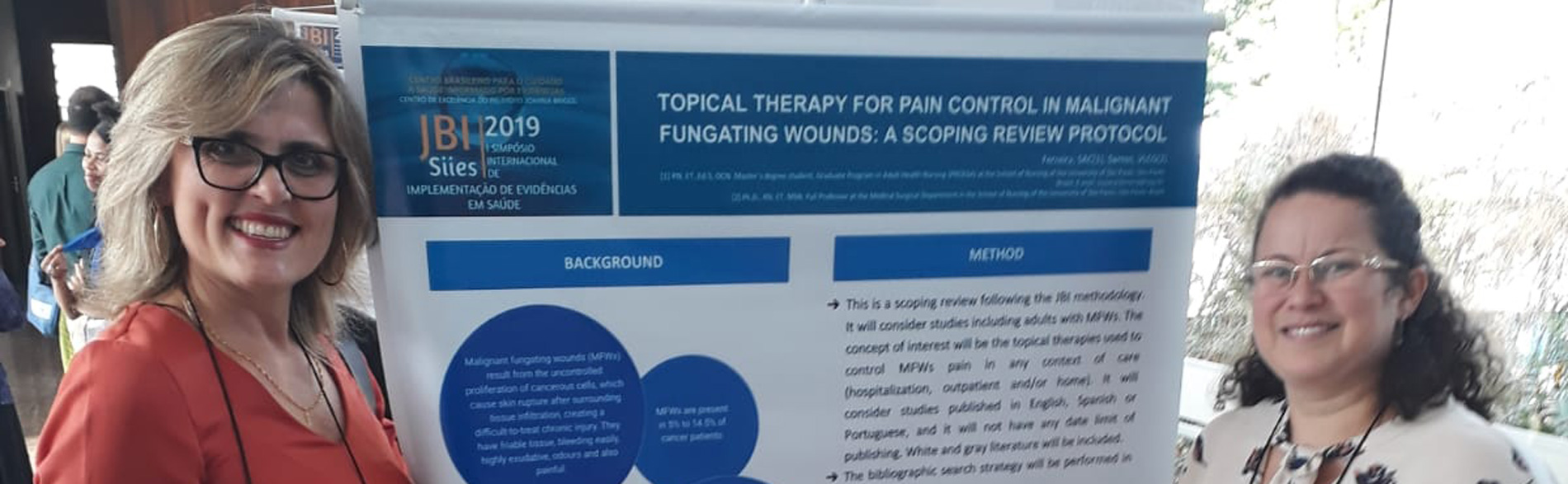
‘Together with a team of nurses participating in the GPET and supervised by Dr. Santos, within the Graduate Program in Adult Health Nursing (PROESA), and supported by JBI Brazil, I carried out a scoping review that aimed to map the existing evidence on topical therapies used to control pain in MFW in accordance with the JBI methodology. The protocol was registered on the Open Science Framework, and presented at the JBI Brazil International Symposium (SIIES, 2019) and finally accepted for publication by Journal Wound Care Latin American.’
Seventy publications were included in the scoping review, comprising 32 non-systematic literature reviews, 20 case studies, six randomised clinical trials, three retrospective cohorts, three systematic reviews, three guidelines, two surveys and a retrospective cohort that showed 20 options for topical therapies for pain control in MFW, categorized as: topical therapies applied in MFW (dressings, analgesic drugs, antimicrobial substances, cryotherapy and negative pressure wound therapy) and skin protectors applied to peri-wound skin.
‘The majority of the topical therapies emerged from non-systematic reviews and case studies which highlighted the need for further studies with more robust designs. However, we found few primary studies evaluating the effectiveness of different interventions, with methodologies considered adequate to support clinical practice.’
The scoping review contributed to the systematisation of the currently available topical therapy options for pain control in MFW, and to mapping knowledge gaps for future research.
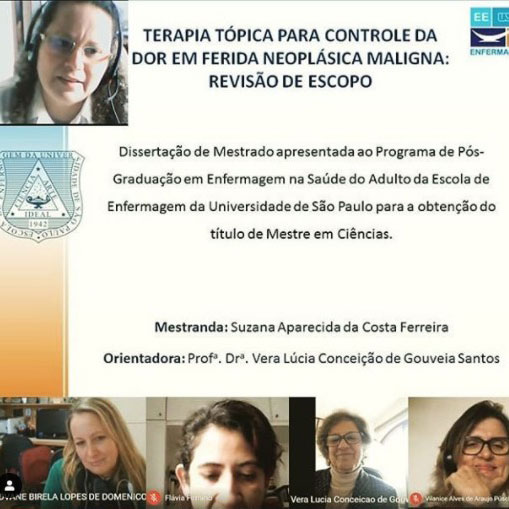
‘The results were presented at an online event to defend my master’s degree, in which many oncology nurses participated. One of these nurses said, “These results are essential to start treating pain topically in our patients with malignant wounds, considering many hospitals do not have any protocol for that purpose”.’
As a result of the scoping review, protocols for managing pain of MFW at Cruz Azul Hospital will be updated according the latest and best available evidence. Currently, a partnership with the National Cancer Institute (INCA) is being explored to update Brazilian national guidelines, and the GPET has partnered with the National University of Colombia to conduct an systematic review of effectiveness and a randomised clinical trial, based on the findings of the scoping review. ‘We believe that the best care is that supported by the best scientific evidence.’
Further resources
- da Costa Ferreira SA, de Gouveia Santos VLC. Topical therapy for pain management of malignant fungating wounds: a scoping review protocol 2020. Open Science Framework. Available at: osf.io/gkv9s.
- Ferreira SAC, Santos VLCG. Topical therapy for pain control in malignant fungating wounds: a scoping review protocol. In: JBI Brasil SIIES 2019. I Simpósio Internacional de Implementação de Evidências em Saúde (SIIES), 2019, São Paulo. v. 1. Available from: https://proceedings.science/siies-2019/papers/topical-therapy-for-pain-control-in-malignant-fungating-wounds--a-scoping-review-protocol
Authors
Suzana Aparecida da Costa Ferreira1
Carol Viviana Serna González1
Adriane Aparecida da Costa Faresin2
Talita dos Santos Rosa1
Magali Thum1
Vera Lúcia Conceição de Gouveia Santos3
1. Graduate Program in Adult Health Nursing-PROESA, School of Nursing of the University of Sao Paulo-EEUSP, Sao Paulo, Brazil
2. Institute of Cancer of Sao Paulo State (ICESP) of Clinics Hospital from the Faculty of Medicine of the University of Sao Paulo (HCFMUSP), Sao Paulo, Brazil
3. Medical-Surgical Department, School of Nursing of the University of Sao Paulo-EEUSP, Sao Paulo, Brazil


References
1. EONS. Recommendations for the care of patients with malignant fungating wounds. Eur Oncol Nurs Soc. 2015;30.
2. Vardhan M, Flaminio Z, Sapru S, Tilley CP, Fu MR, Comfort C, et al. the microbiome, malignant fungating wounds, and palliative care [Internet]. Front Cell Infect Microbiol. 2019;9:373.
3. Robinson PJ, Holloway SL. Psychological factors associated with malignant fungating breast wounds. J Eur Wound Manag Assoc. 2019;20(2):19–23.
4. Willis S, Anstey S. Compassionate leadership in district nursing: a case study of a complex wound. Br J Community Nurs. 2019;24(2):50–7.
5. Beretta L de L, Santos MLSC dos, Dos Santos WA, Fuly PC, Berardinelli LMM. Resiliência no processo do cuidado aos pacientes com feridas tumorais malignas: revisão integrativa. Res Soc Dev. 2020 Mar 20;9(4):117942922.
6. Thomaz A. Dor oncológica: conceitualização e tratamento farmacológico. Onco&. 2010;agosto/set:24–9.
7. Gibson S, Green J. Review of patients’ experiences with fungating wounds and associated quality of life. J Wound Care. 2013;22(5):265–75.
8. Firmino F, Ferreira SA da C, Franck EM, Queiroz WMS de, Castro DLV, Nogueira PC, et al. Malignant wounds in hospitalized oncology patients: prevalence, characteristics, and associated factors. Plast Surg Nurs. 2020;Epub before print.
9. LeBon B, Zeppetella G, Higginson IJ. Effectiveness of topical administration of opioids in palliative care: a systematic review. J Pain Symptom Manage. 2009;37(5):913–7.
10. Graham T, Grocott P, Probst S, Wanklyn S, Dawson J, Gethin G. How are topical opioids used to manage painful cutaneous lesions in palliative care? A critical review. Pain. 2013;154(10):1920–8.
11. Finlayson K, Teleni L, McCarthy AL. Topical opioids and antimicrobials for the management of pain, infection, and infection-related odors in malignant wounds: a systematic review. Oncol Nurs Forum. 2017;44(5):626–32.
12. Adderley UJ, Holt IGS. Topical agents and dressings for fungating wounds. Cochrane Database Syst Rev. 2014;2014(5).
Disclaimers
The views expressed in this this World EBHC Day Impact Story, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.