Strengthening guideline development and implementation for paramedics in South Africa

Successfully developing and implementing guidelines requires a clear understanding of local contextual barriers, the perceptions of the guideline end-users, and possible solutions to any issues that may arise in these scenarios.
In 2016, the first evidence-based prehospital clinical practice guideline1 (CPG) was developed for South African paramedics, replacing outdated and eminence-based practice protocols, and implemented nationally. However, they have had vast implications for paramedic education, practice and service delivery.
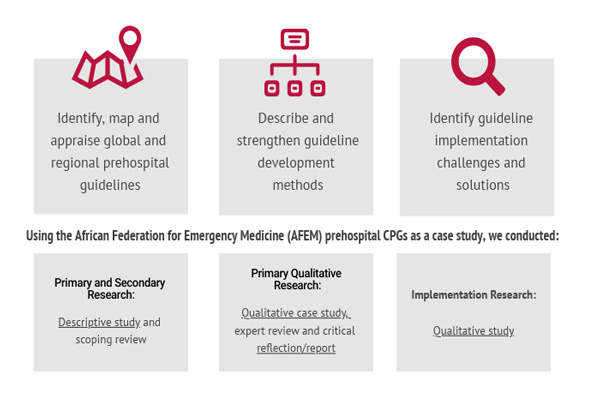
Despite developing guidelines based on the best available evidence, their implementation has not been easy for decision-makers. In response to this, researchers from the Centre for Evidence-based Health Care at Stellenbosch University in South Africa, together with key decision-makers, asked paramedics how to strengthen the uptake of these new guidelines. This research was part of a larger project2 aimed to strengthen the development and implementation of paramedic CPGs in South Africa.
Michael McCaul is a senior lecturer at the Division of Epidemiology and Biostatistics at Stellenbosch University in South Africa. He is a clinical epidemiologist and biostatistician, with a clinical background as an emergency care practitioner, having worked as a paramedic in South Africa for many years. ‘I remember sitting in the back of the ambulance, being utterly frustrated at the lack of treatment options available, and being ill equipped to motivate for change. From that day, I started the journey to contribute to evidence-informed healthcare and decisions.’
Michael has a particular interest in evidence-based healthcare, evidence synthesis and, recently, guideline development. His implementation project focused on exploring and describing paramedics’ perceptions of the CPGs, and understanding barriers and facilitators to guideline implementation. He used qualitative research methods in which, at the research protocol development and funding acquisition stages, key policy decision-makers were involved to provide input and guide knowledge translation. This enabled the research objectives and outputs to be useful and relevant to those who are primarily responsible for the guideline’s policy and implementation action.
Michael and his colleagues conducted focus group interviews with groups of paramedics (from both private and public practice) all over South Africa. Key solutions focused around communication, technology, autonomy and education, highlighting the need for clear and consistent communication from stakeholders, the creation of inclusive career pathways and an end-user document that aids the transition process. They published the results3 and presented at various international and national conferences.
Publishing results in a journal, no matter how high profile or prestigious, simply isn’t enough. Transferring evidence into action and impact is one of the biggest challenges faced by researchers, but this is critical if they are really to make a difference. To enhance impact, Michael’s team used a tailored, audience-specific knowledge translation approach by a priori defining the who (audience), why (purpose), what (message), how (medium/forum), when (timing) and the cost (resources). These knowledge translation activities are summarised in the following matrix.
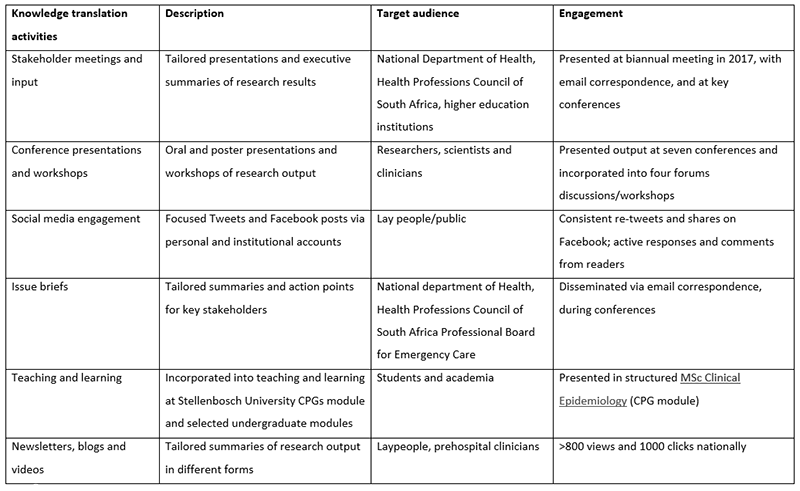
The team used a variety of media to disseminate the information, such as infograms via social media, national newsletters, YouTube videos (for paramedics), research summaries and linking with emergency medicine bloggers #BadEM, and importantly, providing issues briefs for key role players, specifically the South African National Department of Health and the Health Professions Council of South Africa Professional Board of Emergency Care (HPCSA PBEC).
We were pleased to see several indicators of use and impact:
- key findings were shared and presented at agenda-setting national meetings;
- evidence was used and cited by the national guideline implementation task team established to provide recommendations to the HPCSA PBEC for successful guideline implementation and uptake.
Although not empirically measured and difficult to determine, many of the current implementation activities in South Africa are linked to priority actions and recommendations shared with the national decision-makers. These include:
- implementation of online CPG update courses;
- development of a CPG handbook;
- increased communication and transparency from stakeholders.
Supporting decision-makers to implement the guidelines through research was not without major challenges. During the research, the South African prehospital regulatory, political and educational landscape changed drastically. A new HPCSA PBEC and national director for emergency medical care was appointed and paramedic short courses were closed – all while paramedics were at their most vulnerable due to continuous community attacks on ambulances. As the larger project progressed, so did the political landscape, and important role players, such as the regulators, became increasingly reserved in contributing to research, adding to the challenge of getting evidence where it can have impact.
As Michael says, ‘With regard to strengthening prehospital guideline implementation in the future, I believe my research evidence points to a process whereby guidelines are developed with transparent and deliberate input from those who will be using the guidelines in the end, together with decision-makers.’
Authors
Michael McCaul1, Lynn Hendricks1, Raveen Naidoo2, Taryn Young1, Stevan Bruijns3, Mike Clarke1,4
1. Centre for Evidence-based Health Care, Division of Epidemiology and Biostatistics, Department of Global Health, Stellenbosch University, South Africa
2. Director Emergency Medical Services and Disaster Medicine, National Department of Health, Johannesburg, South Africa
3. Division of Emergency Medicine, University of Cape Town, South Africa
4. Centre for Public Health, Queen’s University Belfast, Northern Ireland, United Kingdom


References
1. McCaul M, African Federation for Emergency Medicine Emergency Care Guideline Project Core Team, de Waal B, Hodkinson P, Grimmer K. South African pre-hospital guidelines: report on progress and way forward. African J Emerg Med. 2016;6(3):113-15.
2. McCaul M, Young T, Bruijins S, Clarke M. Strengthening South African prehospital guidelines: learning from the past, for the future [internet]. n.d. [cited YYYY MMM DD]. Available from: https://infogram.com/1to0zeoew89rxphx47d69wl748b11qoq02q.
3. McCaul M, Hendricks L, Naidoo R. Prehospital providers’ perspectives for clinical practice guideline implementation and dissemination: strengthening guideline uptake in South Africa. PLOS One. 2019;14(7): e0219761.
Disclaimers
The views expressed in this this World EBHC Day Impact Story, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.