Reinventing the Belgian evidence-based practice landscape: The example of Evikey
World EBHC Day 2024 provides a unique platform to rethink our approach to human and global health. To drive large-scale change, it is essential to reconsider how different stakeholders—public, policymakers, and the private sector—interact. The Belgian Evikey network serves as an excellent example of how a solid, participative governance model can foster multidisciplinary collaboration in health care.
Introduction
For many years, various organizations in Belgium have promoted evidence-based practice (EBP) within primary care. However, before Evikey, these initiatives lacked coordination and consistency. Although there was good dissemination of EBP, there was limited focus on targeted actions to promote EBP directly. Furthermore, many initiatives were primarily aimed at general practitioners, overlooking the multidisciplinary nature of modern health care.
Evikey was established to bridge this gap and foster a robust EBP culture throughout Belgium's health care system.
Background
A ministerial briefing shed light on the implementation of EBP in Belgium. The report showed the fragmented nature of the EBP landscape, the funding mechanisms, as well as the insufficient uptake by end-users.
In response to these findings, several key actions have been initiated:
1. The creation of a federal EBP governance plan for primary care, with potential future expansion to secondary care.
2. The identification, harmonization, and validation of current EBP stakeholders and activities.
3. A focus on implementation and evaluation efforts.
4. Initiatives to improve the overall effectiveness and efficiency of EBP.
These measures aim to enhance the coherence and impact of EBP in Belgium by ensuring better coordination and more rigorous implementation across the health care system.
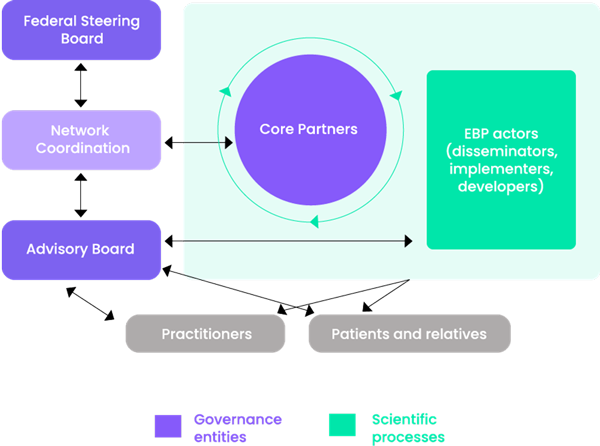
A participatory governance model and collaborative decision-making
Evikey’s governance is founded on the active participation of all stakeholders involved in the EBP process. Operating under collaborative decision-making principles, the network embraces a participatory approach, where decisions are made by consensus. This encourages collaboration and shared responsibility across the board.
Three core entities drive this governance structure:
1. Core partners: These partners are at the heart of Evikey’s scientific activities, ensuring seamless interaction between different phases of the EBP lifecycle and the health care field. Further information about them can be found in the section entitled “The EBP Lifecycle: The Value of the Network.”
2. Federal Steering Board: Comprising representatives from the Belgian National Institute for Health and Disability Insurance (INAMI-RIZIV), the Federal Public Service for Public Health, the Minister of Health, the Belgian Health Care Knowledge Centre, and the Federal Agency for Medicines and Health Products, this steering board provides strategic direction. It validates decisions from the Core Partners and the Advisory Board, while also coordinating EBP efforts at the federal level.
3. Advisory Board: This committee includes practitioners, patients, “mutuelles,” and EBP stakeholders. It plays a crucial role in advising the network, ensuring that its strategies are informed by real-world health care needs.
This governance structure promotes a bottom-up approach, ensuring that health care professionals, patients, and other key stakeholders are actively involved in all initiatives. As a result, Evikey is able to develop solutions that are both practical and sustainable, reflecting the diverse needs and expectations of the community.
The EBP lifecycle : The value of the network
The EBP lifecycle at Evikey follows a structured, sequential process that ensures the ethical and effective use of evidence at every stage. Each phase, coordinated by one of our Core Partner organizations, is essential to guaranteeing the quality of EBP information and addressing the most pressing health care issues (refer to the diagram below).
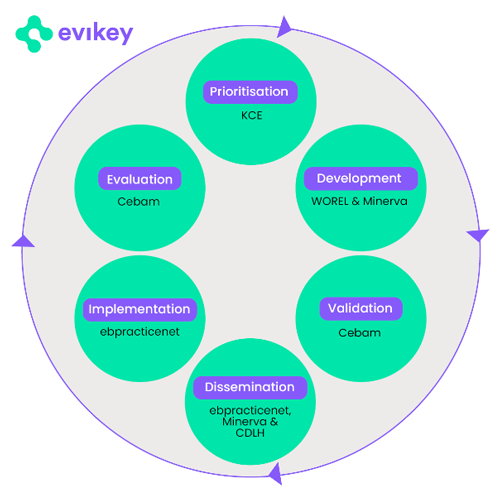
1. Prioritization: This phase, managed by the Belgian Health Care Knowledge Centre, involves identifying and prioritizing research topics with the highest potential for improving health care quality.
2. Development: Two Core Partners, WOREL (The Working Group Development of Primary Care Guidelines) and Minerva, work on developing clinical guidelines and analyzing current medical literature. Together, they contribute to the creation of "Living Guidelines," which evolve as new evidence emerges.
3. Validation: The Belgian Centre for Evidence-Based Medicine (CEBAM) oversees the validation phase, ensuring the scientific integrity of the guidelines. CEBAM also offers training to health care professionals.
4. Dissemination: Evikey Core Partners, ebpracticenet and the CEBAM Digital Library for Health, ensure that EBP guidelines and other materials are effectively shared with health care providers. Most of this information is offered free of charge.
5. Implementation: During this phase, Evikey supports health care providers in integrating EBP into their daily practices. Ebpracticenet plays a key role in this process.
6. Evaluation: The final phase involves assessing the impact of the initiatives and determining whether to continue or restart the cycle. CEBAM leads this evaluation by gathering feedback and measuring outcomes.
Collaborative efforts to improve health
Evikey’s initiatives are funded by the Belgian government, reflecting the unique model of collaboration between scientists, government agencies, and health care providers. This cooperative approach, where all parties work toward a shared goal, is central to Evikey’s success.
The collaboration to enhance EBP in health care operates on several levels:
- Policy level: At this level, key health care themes are addressed. The government provides a framework, while scientists, health care professionals, and other stakeholders further develop it by considering practical needs. Evidence-based interventions are implemented to improve the efficiency of care.
- Content level: Expertise from various areas is integrated. For instance, when a clinical guideline is developed, an accompanying implementation plan is created using insights from implementation science. Indicators are also designed to monitor the impact of these guidelines.
- Interdisciplinary level: A multidisciplinary approach to care is promoted, encouraging the adoption of an evidence-based culture among health care providers. This is facilitated through collaboration with EBP experts to support ongoing improvements in practice.
This multi-level collaboration ensures that EBP is effectively integrated into health care, improving both policy and practice.
Conclusion
The Evikey network is a perfect example of the transformative impact of strong, participatory governance in the health care sector. By engaging health care professionals, patients, and other stakeholders, Evikey has successfully fostered a multidisciplinary collaboration that enhances care quality and addresses the real needs of the population.
Key takeaways
Network organizations provide numerous benefits, including flexibility and the capacity to adapt to change. However, their success hinges on strong coordination, clear agreements, and the ability to collaborate effectively, even when perspectives differ.
- Fostering multidisciplinary collaboration: By promoting partnerships among scientists, health care providers, policymakers, and local communities, Evikey ensures health care is patient-centered and responsive to real health challenges.
- Adopting an inclusive approach: Engaging a broader range of disciplines and stakeholders from the outset allows for a more comprehensive and holistic approach to health care.
- Uniting around a common goal: The network has unified various EBP organizations and centers of expertise, streamlined their working methods, amplifying their collective influence in ways that would not have been possible individually.
References
Evikey. https://www.evikey.be/en/
Vriesacker, K., Adriaenssens, J., Sonnaert, M., Jonckheer, P., Van Bruystegem, E., & Eyssen, M. (2019). Charter of good governance. Belgian EBP Network. https://www.evikey.be/en/resources/
Adriaenssens, J., Benahmed, N., Eyssen, M., Paulus, D., & Mertens, R. (2018). Towards an integrated evidence-based practice plan in Belgium – Part 1: literature, Belgian situation and end-user needs. Health Services Research (HSR). Brussels: Belgian Health Care Knowledge Centre (KCE). KCE Reports 291. D/2018/10.273/12.
Vriesacker, K., Cambré, B., Kokkeler, B., van der Kamp, B., de Goeij, H., Terrier, A., Eyssen, M., & Adriaenssens, J. (2018). Towards an integrated evidence-based practice plan in Belgium – Part 2: Governance Plan. Health Services Research (HSR). Brussels: Belgian Health Care Knowledge Centre (KCE). KCE Reports 291. D/2018/10.273/13.
To link to this article - DOI: https://doi.org/10.70253/FBTV2578
Disclaimer
The views expressed in this World EBHC Day Blog, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.
