Embedding collaborative priority-setting and adaptation in WHO’s evidence ecosystem
Authors: Trudy D Leong1, Emmanuel Effa2, Nyanyiwe Mbeye3, Claire Glenton4 and Tamara Kredo1
1. Health System Research Unit, South African Medical Research Council, Cape Town, South Africa
2. Cochrane Nigeria, Institute of Tropical Diseases Research and Prevention, University of Calabar Teaching Hospital, Calabar, Nigeria
3. Evidence Informed Decision-making Centre, Department of Community and Environmental Health, School of Global and Public Health, Kamuzu University of Health Sciences, Blantyre, Malawi
4. Department of Health and Functioning, Western Norway University of Applied Sciences, Bergen, Norway
Evidence is powerful—but only if it can be translated into action. For many countries, particularly in low- and middle-income contexts, the challenge is not a lack of global evidence, but rather making that evidence relevant, feasible and sustainable at the local level.
This World EBHC Day, we reflect on how collaboration across countries, ministries, researchers and global institutions is helping to close this gap. A key initiative is the Global Evidence, Local Adaptation (GELA) Project, a three-year project working alongside Ministries of Health in South Africa, Nigeria and Malawi.
Why Global Evidence Needs Local Collaboration
The World Health Organization (WHO) has invested in key tools to support evidence-informed health policy:
- EVIPNet: building institutional capacity for knowledge translation.
- WHO-CHOICE: providing comparative cost-effectiveness analysis.
- ADOPT/ADAPT Framework: supporting the contextualisation of guidelines.
- WHO Guidelines: ensuring methodological rigour.
- WHO Ethics Guidance (2025): embedding justice, transparency and inclusivity in decision-making.
Each tool is valuable, but they are often used in isolation, reactively and within short project cycles. This limits their long-term impact and often leaves ministries with fragmented rather than integrated support.
This is where collaboration becomes critical, not just among global and local partners, but also across tools, processes and programs.
GELA: Building bridges, not duplicates
The GELA Project (2022–2025) takes a distinctive approach. Instead of waiting for global evidence to ‘trickle down,’ GELA starts with national priority-setting, co-led by Ministries of Health.
Examples of GELA’s work include:
- South Africa: prioritising anaemia prevention and post-discharge family support.
- Nigeria: improving feeding practices for low birthweight infants and hand hygiene among health workers.
- Malawi: enhancing nutrition in critically ill children.
Beyond identifying priorities, GELA brings together multiple streams of evidence (clinical, economic, contextual and implementation data) using tools like the GRADE Evidence-to-Decision framework and the TRANSFER approach. Crucially, it embeds capacity-building and mentorship over several years, ensuring ministries are not just recipients of evidence but co-producers.
Perhaps most distinctively, GELA explicitly attempts to operationalise ethical principles such as justice, inclusivity and transparency, reflected in structured, documented and equitable decision-making processes.
Collaboration in action: A synergised ecosystem
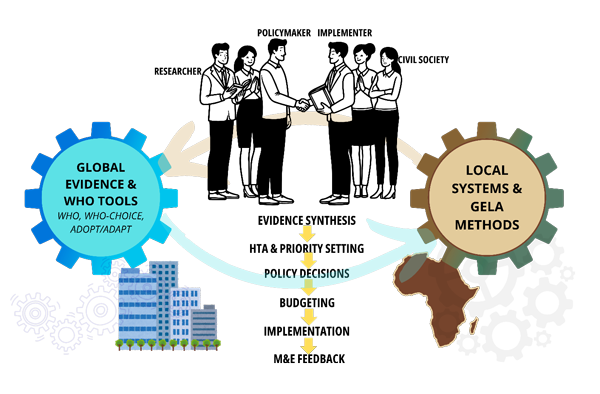
When seen together, the WHO tools and GELA methods are not competitors but complementary approaches. The evidence-to-policy process can be conceptualised as a continuous, collaborative cycle:
1. Priority setting with Ministries of Health (GELA + WHO Ethics Guidance).
2. Economic modelling for cost-effectiveness (WHO-CHOICE).
3. Guideline contextualisation (ADOPT/ADAPT Framework + digital platforms).
4. Institutional translation into policies and briefs (EVIPNet).
5. Monitoring, evaluation and adaptation (GELA’s iterative approach).
This integrated workflow attempts to transform fragmented use of evidence into a cohesive, ongoing, iterative, inclusive, collaborative ecosystem. It also creates space for global standards to align with local realities, while maintaining rigour, equity and sustainability.
What this means for policy and practice
Collaboration is not just a theme; it’s a practical necessity.
- For WHO: possibly promote integrated toolkits that combine existing initiatives with GELA’s structured, cyclical approach.
- For Ministries of Health: the priority is to invest in sustained, ethical evidence processes, not just one-time projects.
- For donors: the opportunity lies in supporting long-term systems that build national capacity and ensure lasting impact.
Conclusion: Collaboration as the key element
The GELA Project illustrates that the future of evidence-informed policy is not just about inventing new tools – it’s about collaboration. The GELA approach is still a work in progress and will benefit from continued refinement and learning through implementation. However, by embedding priority-setting, adaptation and ethical principles of engagement, inclusivity and legitimacy into the WHO’s broader ecosystem, GELA offers a pragmatic bridge between global evidence and local action.
On this World EBHC Day, we are reminded that collaboration is the cornerstone of equity and sustainability in health policy. The real opportunity ahead lies in working together – governments, donors, researchers and global institutions – to embed and synergise what we already have. Because when collaboration is at the centre, evidence can effectively transform health systems and support universal health coverage.
References
Bertram, M.Y. & Edejer, T.T.T., 2021. Introduction to the special issue on ‘The World Health Organization Choosing Interventions That Are Cost-Effective (WHO-CHOICE) update’. International Journal of Health Policy and Management, 10(11), pp.670–672. doi: 10.34172/ijhpm.2021.105.
Booth, A., Moore, G., Flemming, K., Garside, R., Rollins, N., Tunçalp, Ö. & Noyes, J., 2019. Taking account of context in systematic reviews and guidelines considering a complexity perspective. BMJ Global Health, 4(Suppl 1), p.e000840. doi: 10.1136/bmjgh-2018-000840
Durão, S., Effa, E., Mbeye, N., Mthethwa, M., McCaul, M., Naude, C. et al., 2024. Using a priority setting exercise to identify priorities for guidelines on newborn and child health in South Africa, Malawi and Nigeria. Health Research Policy and Systems, 22(1), p.48. doi: 10.1186/s12961-024-01133-7.
Kredo, T., Durão, S., Effa, E., Naude, C., McCaul, M., Brand, A. et al., 2024a. Building sustainable capacity to adopt, adapt or develop child health guidelines, Malawi, Nigeria and South Africa. Bulletin of the World Health Organization, 102(10), pp.749–756. doi: 10.2471/BLT.24.291564.
Kredo, T., Effa, E., Mbeye, N., Mabetha, D., Schmidt, B.M., Rohwer, A. et al., 2024b. Evaluating the impact of the Global Evidence, Local Adaptation (GELA) project for enhancing evidence-informed guideline recommendations for newborn and young child health in three African countries: a mixed-methods protocol. Health Research Policy and Systems, 22(1), p.114. . doi: 10.1186/s12961-024-01189-5.
Moberg, J., Oxman, A.D., Rosenbaum, S., Schünemann, H.J., Guyatt, G., Flottorp, S. et al., 2018. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions. Health Research Policy and Systems, 16(1), p.45. doi: 10.1186/s12961-018-0320-2.
Munthe-Kaas, H., Nøkleby, H., Lewin, S. & Glenton, C., 2020. The TRANSFER approach for assessing the transferability of systematic review findings. BMC Medical Research Methodology, 20(1), p.11. doi: 10.1186/s12874-019-0834-5.
Schmidt, B.M., Mabetha, D., Chibuzor, M., Kunje, G., Arikpo, D., Aquaisua, E. et al., 2024. Developing and planning country-specific integrated knowledge translation strategies: experiences from the GELA project in Malawi, Nigeria and South Africa. BMC Public Health, 24(1), p.1418. doi: 10.1186/s12889-024-18934-8.
World Health Organization, 2023. Strengthening countries’ capacities to adopt and adapt evidence-based guidelines: a handbook for guideline contextualization. Copenhagen: WHO Regional Office for Europe. Licence: CC BY-NC-SA 3.0 IGO. Available from: https://reliefweb.int/attachments/94a6afed-c740-4d10-8c6e-9f3cea4f0f44/9789289060028-eng.pdf [Accessed 22-08-2025]
World Health Organization, 2021. Evidence, policy, impact. WHO guide for evidence-informed decision-making. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IG. Available from: https://www.who.int/publications/i/item/9789240039872 [Accessed 22-08-2025]
World Health Organization, 2025. WHO guidance on the ethics of health research priority setting. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. Available from: https://iris.who.int/bitstream/handle/10665/381711/9789240110953-eng.pdf [Accessed 22-08-2025]
World Health Organization. 2014. WHO handbook for guideline development, 2nd ed. Available from: https://iris.who.int/handle/10665/145714 [Accessed 22-08-2025]
To link to this article - DOI: https://doi.org/10.70253/LBSU2398
Disclaimer
The views expressed in this World EBHC Day Blog, as well as any errors or omissions, are the sole responsibility of the author and do not represent the views of the World EBHC Day Steering Committee, Official Partners or Sponsors; nor does it imply endorsement by the aforementioned parties.
